Expanding Medicare to cover weight loss drugs would cost $35 billion over eight years, according to a new report from the Congressional Budget Office (CBO).
In its estimates released Tuesday, CBO said 12.5 million Medicare beneficiaries would qualify for the medications beginning in 2026, and 2 percent would be expected to use the drugs in the first year.
The nonpartisan scorekeeper found that relative to the direct costs of the medications, “total savings from beneficiaries’ improved health would be small.” The direct federal cost to cover the drugs would increase from $1.6 billion in 2026 to $7.1 billion by 2034.
BestReviews is reader-supported and may earn an affiliate commission.
Best Prime Day 2024 Deals
Don’t miss the best sales of Prime Big Deal Days
According to CBO, savings would be less than $50 million in 2026 and rise to $1 billion in 2034. Average prices for the drugs are projected to fall by increasing amounts in the second decade, but federal spending would still rise through 2044.
CBO estimated the policy would apply to all beneficiaries with obesity, as well as certain beneficiaries who are classified as overweight. More than two-thirds of Medicare beneficiaries are classified as either obese or overweight, according to their body mass index.
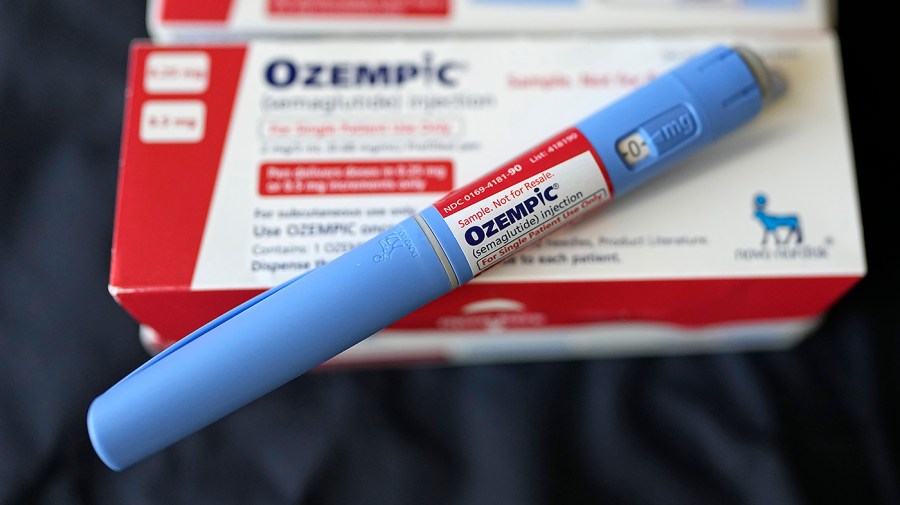
Medicare is currently prohibited from covering anti-obesity medication or Ozempic, unless they are also approved for diabetes and cardiovascular disease. The CBO report comes as lawmakers debate how to cover the popular, but extremely expensive, treatments, which can cost upwards of $1,000 a month.
The CBO report was not scoring a specific bill, but rather an illustrative example of a policy.
In June, the House Ways and Means Committee overwhelmingly passed legislation to expand Medicare coverage of weight loss drugs, but it was a narrowly tailored bill aimed at ensuring people who are already taking the drugs don’t lose access if they enroll in Medicare. It would limit coverage to people who had been taking a weight loss drug for a year prior to enrolling in Medicare.